Implantation
- Interaction between an embryo and the endometrium
This process seems to be affected by two crucial factors ;
- Endometrial receptivity
- Synchronization between the embryo developmental stage and endometrial profile during the window of implantation
Endometrial receptivity needs
- 2 hormons;
- Estrogen and progesterone
- An important factor in the process of embryo implantation is endometrial receptivity and synchronisation between embryonic and endometrial development.
Keypoints in performing FET
- Selecting proper embryos used for FET
- Accurate synchronization of endometrium and embryos
- Sufficient luteal support
Endometrial preperation & FET
- Timing of embryo transfer is determined by detecting the spontaneous LH surge or by administering hCG to initiate luteinization
- A frequently employed alternative approach is represented by ‘artificial cycle protocols’ in which exogenous estrogens and progesterones are administered, with or without co-treatment with GnRH agonists
Protocols for endometrial preperation
- Naturel cycle
- Naturel cyle + hCG (Modified NC)
- Ovulation induction (CC, Letrozol, Gnd) + hCG
- Artificial cycle FET (AC-FET)
- –GnRh-a programmed with E2 and P administration
- –Non GnRh-a programmed with E2 and P administration
Naturel Cycle in FET
- Women with regular cycles (Ovulatory cases)
- Cheaper
- May be used in young cases
- It is not proper option when better control and flexibility in timing is desired
- It requires endogeneous hormon production
- Ovulation time must be identified clearly
- This may cause anxiety, Cancel rate %6
Naturel Cycle in FET
- It can not be used in;
- Menstrual irregularity
- PCOS, anovulation, LPD prevents clear determination of ET time
- CC, Letrozol and Gnd can be used for timing of ovulation and ET
Naturel Cycle & technique
- 4 days before ovulation, monitorization starts D 8-9
- DF > 14 mm LH measurement
- Progestereron support is not usually required, sometimes P may be given for luteal support
Naturel Cycle & technique
- In order to assess the LH levels correctly, determination should be performed at least daily, and preferably twice a day.
- LH urine kits have a large variation in thresholds, which involve the risk of up to 30% of false-negative testing, and are often reported by patients as being difficult to interpret
Miller and Soules, 1996; Guermandi et al., 2001; O’Connor et al., 2006
modified NC-FET
- To overcome the disadvantages of LH monitoring, hCG triggering of ovulation is often employed in NC-FET in what is termed ‘modified NC-FET’.
- This approach does not require LH monitoring but regular ultrasound evaluation of the dominant follicle is required to ensure appropriate timing of hCG administration.
- As soon as the dominant follicle is of sufficient size (17–18 mm) hCG is administered as a surrogate to the endogenous LH surge to trigger final oocyte maturation and ovulation, which takes place 36–38 h later
Andersen et al., 1995
Artificial cycle FET (AC-FET)
- Estrogen and progesterone are administered in a sequential regimen which aims to mimick the endocrine exposure of the endometrium in the normal cycle.
- Initially, estradiol is given in order to cause proliferation of the endometrium, while suppressing the development of the dominant follicle.
- This is continued until the endometrium is observed to be 7–9 mm thick on ultrasound, at which time progesterone is added to initiate secretory changes
El-Toukhy et al.,2008
Artificial cycle FET (AC-FET)
- The physiological mid-cycle shift from estrogen to progesterone is thus emulated
Dor et al., 1991; Jaroudi et al., 1991
- The timing of embryo thawing and transfer is planned according to the moment of progesterone supplementation
- The administration of estrogen and progesterone does not guarantee complete pituitary suppression, and a dominant follicle may therefore occur.
- Should the follicle undergo spontaneous luteinization then the endometrium may be exposed to progesterone earlier, risking incorrect timing of thawing and transferring
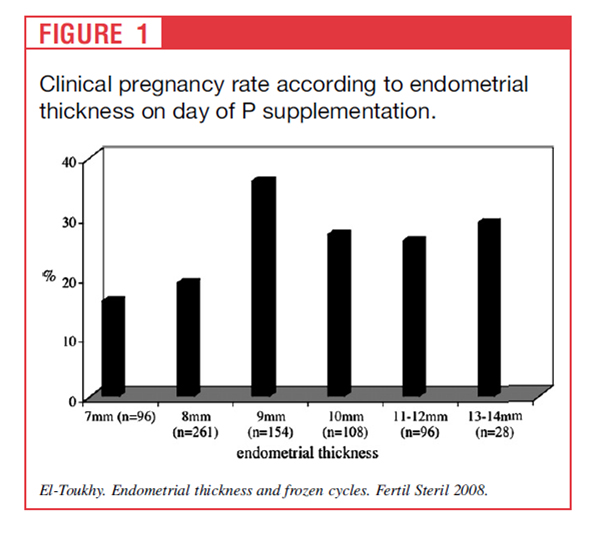
Endometrial thickness and fet outcome
Endometrial thickness
of 9–14 mm before P supplementation is associated with
a higher chance of implantation and pregnancy compared
with a thickness of 7–8 mm
HRT for FET
- E can be given;
- Orally, transdermally, vaginally, sc
- P can be given;
- Orally, IM, vaginally, nasally, rectally, subligually, rectally
- The best route of administration of E and P in preperation for ET is unclear
Combined oral E2 and vaginal P
- Effective
- Simple
- İnexpensive
- Theree is no statistically significant difference between IM and vaginal route of P
HRT in FET (Gn RH-a Programmed)
- HRT is initiated after down regulation
- D1-D8 E2 Valerat or micronized E2 2 mg
- D9-11 4 mg
- D – 12 6 mg
- D 14 USG > 8 mm luteal support
- Micronised P 2 * 400 mg vaginal cap.
- Crinone % 8 (90 mg) vaginal gel
- Cliogest 400 mg vag. tab. 2 * 1
GnRH-a Employment Advantages
- Synchronization between embryo and endometrial development
(anovulation and irregular cycle)
- Decreases the need for USG and hormonal monitorization
- Decreases cancellation rate
- Controlled ET time
GnRH-a Employment Disadvantages
- Prolongation of duration of treatment
- Hypoestrogenic structure
- Flare effect, cyst formation
- GnRH-a for controlled endometrial preperation in FET recipients is not necessary
de Zeigler D 1991, Queenan JT 1997, Simon A 1998, Oborna I 2004
In FET
Significant effect
- Age, number of embryos transferred, embryo quality, endometrial pattern and thickness
No significant effect
- Stimulation type
- Cause of infertility
- Duration of storage
Kondo I, 1996, Avery 1997, Zhu Y, 2001, Kolibianakis EM Jerome HC, 2004
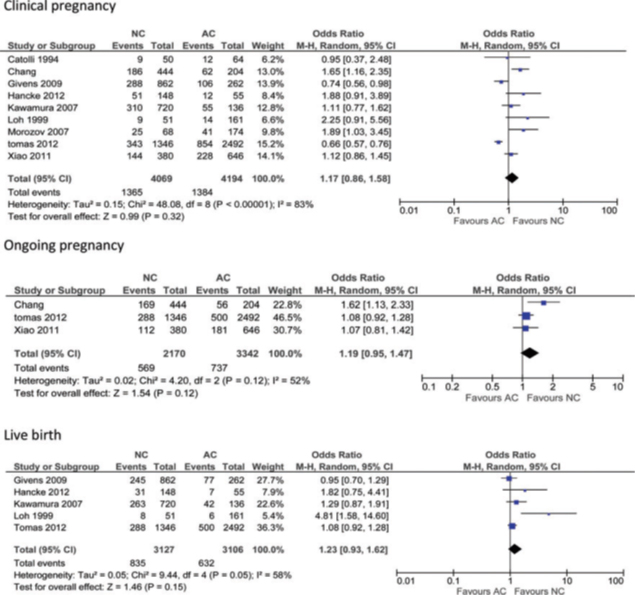
- Despite the growing importance of FET in the treatment of subfertility there is little consensus on the best method for endometrium preparation in ovulatory women
Ghobara and Vandekerckhove, 2008;Weissman et al., 2009
- Recent Cochrane review analysing a number of different protocols used prior to FET, concluded that there is currently no evidence to support the superiority of any one protocol over the other.
Ghobara and Vandekerckhove, 2010
E+P HRT vs Naturale cycle / Klinik gebelik
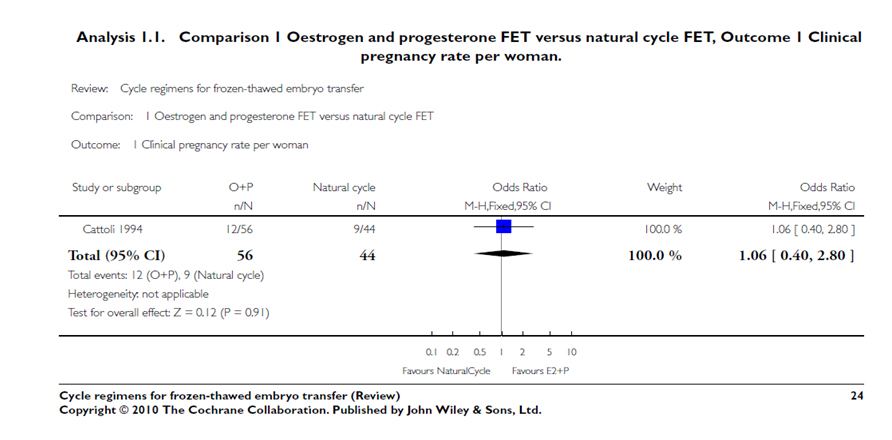
Cochrane 2010
True NC versus modified NC: pooled result of all studies

NC versus AC
NC versus AC with GnRH agonist

AC versus AC with GnRH agonist

Cycle cancellation
- NC-FET poses the risk of unobserved ovulation. If ovulation occurs without notice, accurate planning of embryo thawing and transfer is not possible, which results in cycle cancellation (7–12%)
Fatemi et al., 2010; Hill et al., 2010
- AC-FET does not guarantee complete down-regulation, luteinization may occur in 5% of the cases
El Toukhy et al., 2004
- This meta-analysis revealed no significant advantage of one specific approach to prepare the endometrium for FET in terms of clinical pregnancy rates or live birth rates.
RESULT

CONCLUSION
- Naturel cycle FET and HRT priming FET have equal success
- Endometrial preperation with exogeneous E and P without using GnRH-a is simple,easy, effective and economical in FET cases
- The type and administration route of the steroid form has no effect on the success of the FET cycles
- For decreasing abortion rate in FET cycles;
- vaginal progesterone gel dose administration 180 mg recommended, (2 * 90) morning and late afternoon
- Minimum 12 days Estrogen intake before P
- Blastosist ET at on Day six of P treatment
- Doubling of the progesterone dose in patients receiving endometrial priming with oestradiol and progesterone prior to FET increased the clinical pregnancy rate per transfer and significantly reduced the biochemical pregnancy rate
Orvieto et al. 2007 , Check et al. 2010
- that the viability of an early pregnancy is dependent on a certain threshold of progesterone.
- The unanswered question regards how high the progesterone concentration should be. Interestingly, the concentration does not seem to be constant in all women as visualized in earlier studies, which showed significant histological endometrial differences in patients treated according to the same protocol
Sudoma et al.,2011